Fee-for Service vs. Value-Based Care: A Smarter Future for Healthcare
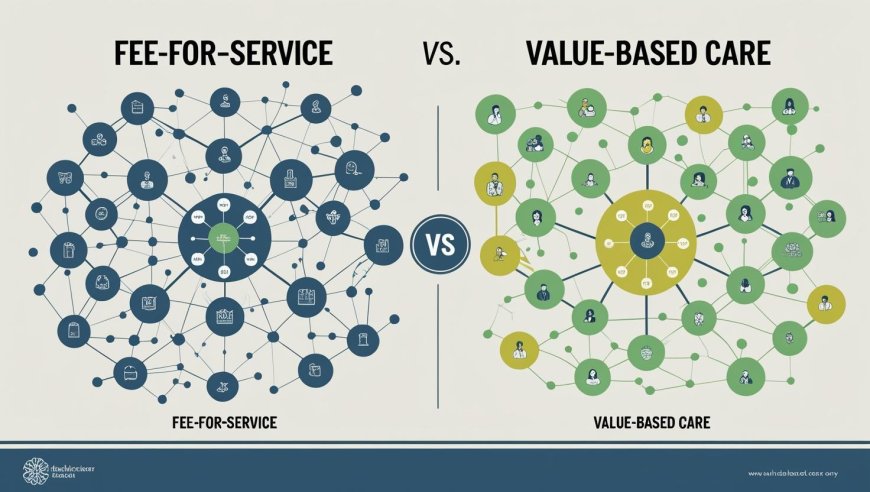
The contrast between value-based and fee-for-service care illustrates the move away from quantity-based payments and toward outcome-driven healthcare. Clinicians who use fee-for-service models are compensated based on the quantity of tests or treatments they do, usually at the expense of long-term outcomes and cost-effectiveness. Value-based care reverses that paradigm by emphasizing cost minimization, better patient health, and quality. Despite its difficulties in implementation, CMS programs and healthcare innovators such as Persivia are supporting VBC as the most patient-centered and sustainable alternative.
Incentives in the healthcare sector urgently need to be realigned. Though it may have contributed to system expansion, the old fee-for-service model resulted in overuse, needless operations, and excessive medical expenses. Stakeholders were forced by these findings to reconsider the financing and delivery of healthcare.
The ongoing shift in healthcare is shaped by the dynamics of Fee For Service vs Value-Based Care, as governments aim to reduce spending and patients seek better outcomes. Performance, responsibility, and teamwork are all highly valued in this new paradigm since they are necessary for contemporary systems to continue to function. Here, technology is essential, and instruments such as a Digital Health Platform enable this development.
The Shift in Healthcare Models
The healthcare industry is undergoing significant change. Fee-for-service was the norm for many years, with clinicians being paid for each visit, scan, and laboratory result. But in the end, the flaws in this system high costs, fragmented treatment, and poor patient outcomes, were revealed. Thus, the shift from fee-for-service vs value-based treatment is one of the most important debates occurring in the healthcare sector today.
Patients want outcomes, not repeat visits. Providers want sustainability, not just volume. And the government and payers want value, not inflated bills. Enter value-based care: a model designed to align payment with quality. Doing better is more important than simply doing more. This shift is now more possible than ever thanks to cutting-edge resources like a digital health platform.
What is Fee-for-Service?
The conventional approach, known as fee-for-service (FFS), pays medical professionals for each service they provide. Every test, examination, or operation has an additional cost. A provider makes more money the more they do.
Why Fee-for-Service Still Exists
-
It's familiar and easy to implement.
-
It offers predictable revenue based on volume.
-
Many insurance systems are built around this model.
Negative aspects of fee-for-service
-
No motivation to concentrate on results.
-
Often results in unnecessary procedures.
-
Promotes fragmented and episodic care.
-
Contributes to administrative overload and stress in clinicians.
What is Value-Based Care?
Caregivers are paid based on patient outcomes, overall care quality, and efficiency under the value-based care (VBC) paradigm. The value offered is the main focus rather than quantity.
Core Features of VBC
-
Emphasizes preventive care and the management of chronic illnesses.
-
Payment is based on performance indicators and results.
-
Promotes cooperation amongst care teams.
-
Provides integrated tracking and reporting through the use of state-of-the-art technologies and a digital health platform.
Real-World Benefits
-
Reduction in hospital readmissions.
-
Better patient satisfaction scores.
-
Increased cost savings for the entire system.
Key Differences Between The Two Models
|
Feature |
Fee-for-Service |
Value-Based Care |
|
Payment Type |
Per service provided |
Based on outcomes |
|
Incentive |
More procedures |
Better results |
|
Patient Focus |
Volume-focused |
Quality-focused |
|
Use of Tech |
Minimal |
Relies on Digital Health Platform tools |
|
Care Coordination |
Low |
High |
|
Risk Sharing |
The provider bears no risk |
Shared financial risk |
Which Model Offers Better Value For Money?
Value-based care has been shown to save billions of dollars over time. For example, the Bundled Payments for Care Improvement (BPCI) model saved around $444 per joint replacement surgery. Meanwhile, Maryland's All-Payer model saved $1.4 billion in five years. Fee-for-service rarely sees these returns because it encourages more care, not necessarily better care.
The CMS Innovation Center continues to expand VBC nationwide through programs like:
-
ACO REACH
-
Comprehensive Primary Care Plus
-
Merit-Based Incentive Payment System (MIPS).
Provider Challenges in Transitioning
Switching to value-based care isn't easy. Many providers face real hurdles:
-
Lack of data infrastructure and analytics tools.
-
Hesitation to accept financial risk.
-
Staff training and workflow redesign.
-
Limited experience with population health models.
Benefits of Value-Based Care
Despite the challenges, VBC offers substantial advantages:
-
Enhanced health results and patient involvement.
-
Simplified communication and coordination of care.
-
Incentives for innovation and efficiency.
-
Long-term cost reduction for payers and systems.
-
Reduced administrative burden through integrated solutions.
How Hybrid Models Are Gaining Ground
For certain treatments, some providers use value-based care instead of fee-for-service, while for other procedures, they use value-based care in addition to fee-for-service. Systems can experiment with new tactics and gain flexibility thanks to these hybrid models without endangering their financial stability.
Through the adoption of the tools and methods necessary for the complete implementation of value-based care, these blended systems enable companies to progressively shift risk.
How Persivia Supports This Transformation
Modern value-based models require digital transformation. This is where Persivia CareSpace comes in. It integrates population health, care management, and quality tracking in one place. Providers can:
-
Use predictive analytics to manage risk.
-
Automate quality reporting and compliance.
-
Monitor results in real time to make better choices.
-
Use insights driven by AI to streamline processes.
Takeaway
In healthcare delivery, value-based care vs fee-for-service represents a paradigm change. Value-based treatment prioritizes results over volume, whereas fee-for-service encourages volume. There are unquestionable advantages in terms of cost control and patient experience, notwithstanding the work needed to implement the shift.
Healthcare businesses may thrive with value-based care thanks to Persivia CareSpace. Persivia makes the move not only feasible but also lucrative with its real-time insights, seamless quality tracking, and end-to-end care coordination.
Take your care delivery to the next level.
Get Started with Persivia Today!